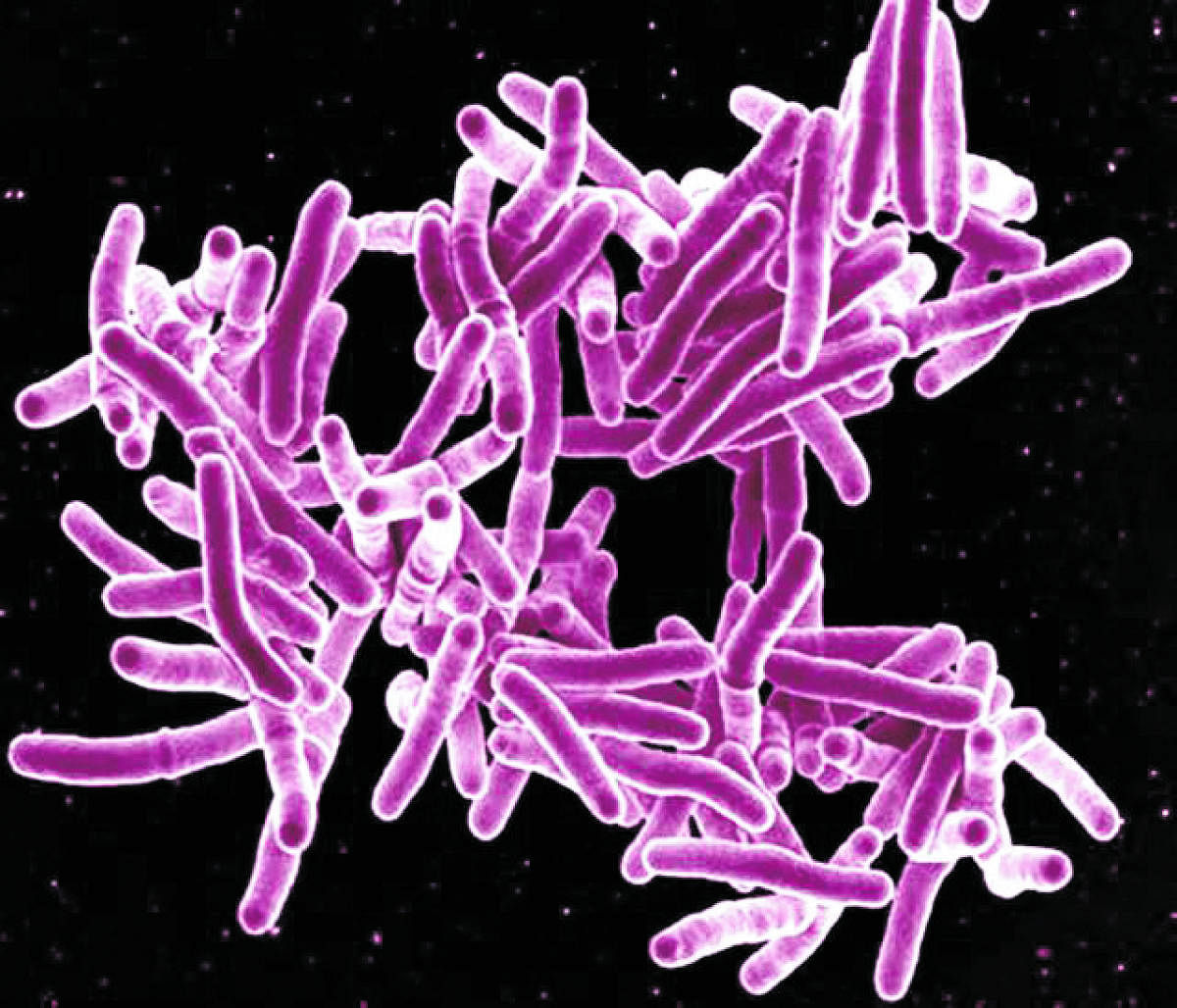
Robert Koch discovered tuberculosis (TB) bacteria nearly 140 years ago, making this one of the earliest diseases to have its causative agent identified by man. Despite this, TB continues to be the leading cause of death due to infectious diseases, infecting over 10 million people annually, and causing over a million deaths. India bears a huge burden of TB, being home to over 25% of all the cases as well as deaths occurring due to it. The last few years have seen a renewed emphasis on the TB programme in India, with the introduction of a new treatment regimen, financial incentives for nutrition support, greater involvement of the private sector, and robust data management. These measures have helped bring attention to the disease, which causes much misery, undernutrition, and deaths. The Covid-19 pandemic has, however, negated many of the hard-won gains.
Since the pandemic began, the detection of new cases has fallen substantially in India. A paper in the Indian Journal of tuberculosis notes that there was a 59% decrease in TB case detection over a period of eight weeks of lockdown in March to May, as compared to the level of detection in the eight weeks just before the lockdown. The data was calculated based on data from the national TB elimination programme.
The authors of the paper, Dr Anurag Bhargava and Dr Hemant Deepak Shewade wrote: “Considering the observed 59% reduction in detection over an eight-week period, there will be an estimated additional 87,711 TB deaths [19.5% increase], bringing the total to 5,37,411 TB deaths in 2020.
In the last five years, 2015 saw the highest number of deaths from tuberculosis at 5,17,000. Since then, the number has been falling, year after year. However, now with these new estimates, the deaths in 2020 will surpass even the 2015 peak. We note that the poor notification of TB cases continues even now: the cases notified from June to September were 67% of those notified in this period a year ago. So, the trend is unchanged even with the progressive easing of the lockdown.
The occurrence and severity of the disease is also closely linked to the nutrition status. Loss of livelihoods and worsening food security will adversely affect nutrition of individuals and could further increase the incidence as well as deaths due to TB.
As physicians, we see the worrying situation on the ground of high occurrence, low detection and poor services for TB management that is likely to fuel an epidemic of TB, especially in rural India.
We work with primary healthcare facilities in rural and tribal areas (in Rajasthan, but this is typical of all India) where public health facilities are poor and erratic.
A patient who presented himself at our clinic many months after he noticed symptoms narrated how he was turned away at PHCs and CHCs. Several other patients have come to us after their treatments were interrupted for durations ranging from one to several months. Many such patients reach us when the disease has advanced substantially. For example, 34-year-old Ramubai came to us with advanced TB and hypoxia. She had sought care at the district hospital and was admitted in a ward for suspected Covid-19 patients for a week. She was discharged after her Covid-19 test was negative, without being further evaluated. Subsequent evaluation revealed she had sputum positive TB and was also HIV positive.
Most health facilities in the area have cut down their outdoor, laboratory and radiology services. In many of these, there is a shortage of drugs, x-ray films and other items. Laboratory technicians are busy testing for Covid-19. Patients are discouraged from walking into facilities and are often not examined or tested. The preoccupation with Covid-19 is leading to the diagnosis of TB being missed on several occasions. Disrupted and erratic transport is making it difficult for patients to reach a health facility, and loss of livelihoods and resultant destitution is making it difficult to afford treatment at a private facility.
Time is running out. With each passing day, more patients are going undiagnosed, and more are dropping out of treatment and developing severe disease. Following are some measures which can help bring the focus back on TB.
Resume and ramp up diagnosis, treatment of TB: While Covid-19 testing and treatment continue, a clear strategy is needed to enable diagnosis and treatment of TB. Dedicated days in the week for testing and initiating treatment at PHCs and CHCs can ensure testing for TB as well as Covid-19. The mandatory CBNAAT test for TB that detects drug resistance requires patients to travel all the way to the district headquarter. In view of the still erratic transport, and scarcity of liquid cash, the sputum samples can be transported rather than patients themselves as is being done now. Additionally, mobile vans with X-Ray facilities can be taken to PHCs.
Promote intake of nutritious foods: Over half of the TB patients are men, the main earning members of the family whose disease severely affects the family’s income and availability of nutritious foods. Malnutrition levels among TB patients are extremely high: In 2019, 93% of all the patients enrolled for treatment at the facilities we manage were undernourished, with 61% being severely so. Poor nutrition in turn adversely affects the disease and the response to treatment. The provision of a cash incentive of Rs 500 per month to patients for their nutrition is a welcome step; the amount is, however, small, and its distribution erratic. The Public Distribution System needs to be made more robust and provide nutritious foods such as pulses and oils in addition to cereals alone, as provided at present. Finally, the anganwadis can expand the coverage of the supplementary food they provide, to include TB patients in addition to women and children.
Generate suitable livelihood options: Extensive lung damage as occurs in many patients limits the scope of their work, even after recovery from TB. Innovative options for livelihoods need to be considered, such as providing guaranteed employment closer home under the NREGS, an important source of rural livelihoods in the present times. Helping patients to set up kitchen gardens and backyard poultry can go a long way in improving the availability of nutritious foods, besides also generating precious income.
As the country continues to count Covid-19 numbers daily, let us shift attention back to the oldest and the most widespread disease. Let us try to reduce the silent suffering, and unknown deaths
(The writers are doctors with Basic Healthcare Services, a non-profit that provides primary healthcare in rural Rajasthan in association with the state government) (Syndicate: The Billion Press)