A government-sponsored clinical trial that is testing an antibody treatment for Covid-19 developed by drugmaker Eli Lilly has been paused because of a “potential safety concern,” according to emails that government officials sent Tuesday to researchers at testing sites. The company confirmed the pause.
The news comes just a day after Johnson & Johnson announced the pause of its coronavirus vaccine trial because of a sick volunteer and a month after AstraZeneca’s vaccine trial was halted over concerns about two participants who had fallen ill after getting the company’s vaccine.
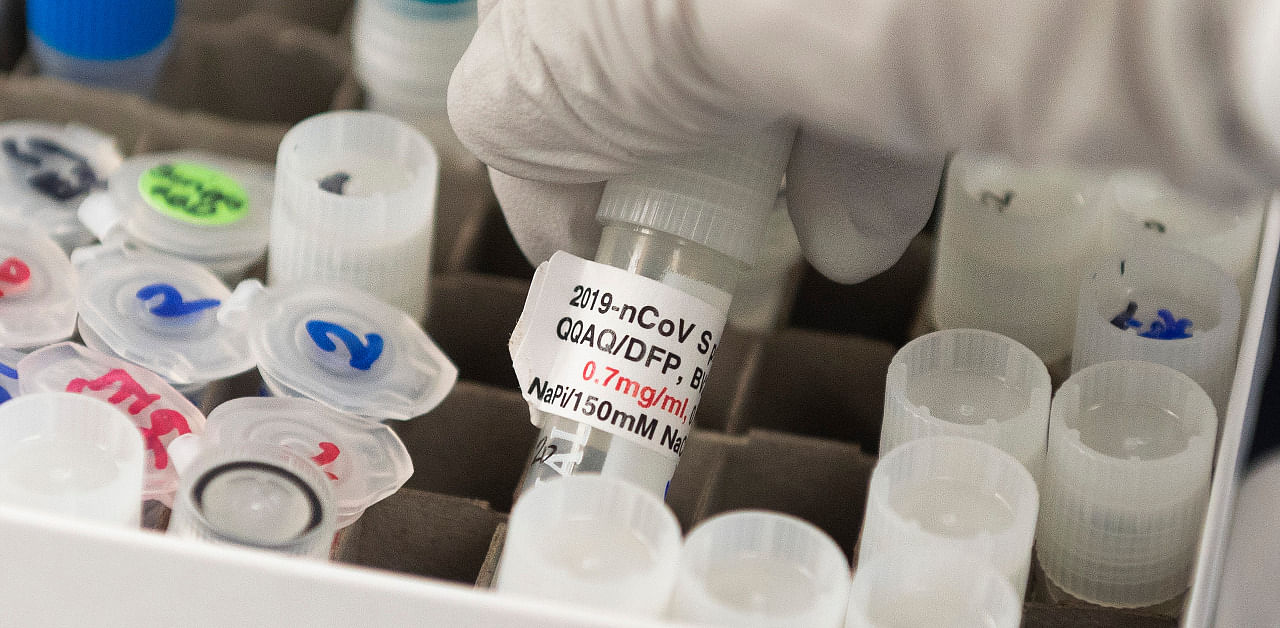
The Eli Lilly trial was designed to test the benefits of the antibody therapy on hundreds of people hospitalized with Covid-19, compared with a placebo. All of the study participants also received another experimental drug, remdesivir, which has become commonly used to treat coronavirus patients. It is unclear exactly what safety issues prompted the pause.
In large clinical trials, such pauses are not unusual, and declines in health in volunteers are not necessarily the result of the experimental drug or vaccine. Such halts are meant to allow an independent board of scientific experts to review the data.
“This is why clinical trials are essential,” said Marion Pepper, an immunologist at the University of Washington. “The safety of the product has to be empirically proven.”
Enrollment for the Eli Lilly trial, which was sponsored by several branches of the National Institutes of Health and the Department of Veterans Affairs, among other organizations, had been continuing. But Tuesday, officials sent emails to researchers telling them to stop adding volunteers to the study out of an “abundance of caution.”
In a statement, an NIH spokeswoman said the trial, which had enrolled 326 Covid-19 patients, was paused when the independent safety board found that after five days of treatment, the group of patients who had received the antibodies showed a different “clinical status” than the group who had received a saline placebo — a difference that crossed a predetermined threshold for safety.
Given the ambiguity in the statements released on Tuesday, all scenarios remain possible, said Dr Eric Topol, a clinical trials expert at the Scripps Research Institute. “It’s so amorphous,” Topol said.
The safety board will review the data again on October 26, and advise the NIH on whether to resume the trial, the statement said. In the meantime, researchers will continue to collect data from people already enrolled in the study.