Roadblocks in organ donation: What’s the way forward?
Three decades after India brought in a new law to facilitate organ donation, the ground realities are starkly different from what the legislation intended to achieve. It was presumed that the law, by recognising brain-death, would aid deceased organ donation in public hospitals. Instead, organ transplantation flourished mostly in the private sector and that too because of living donor transplants, in which an organ is donated by a living individual.
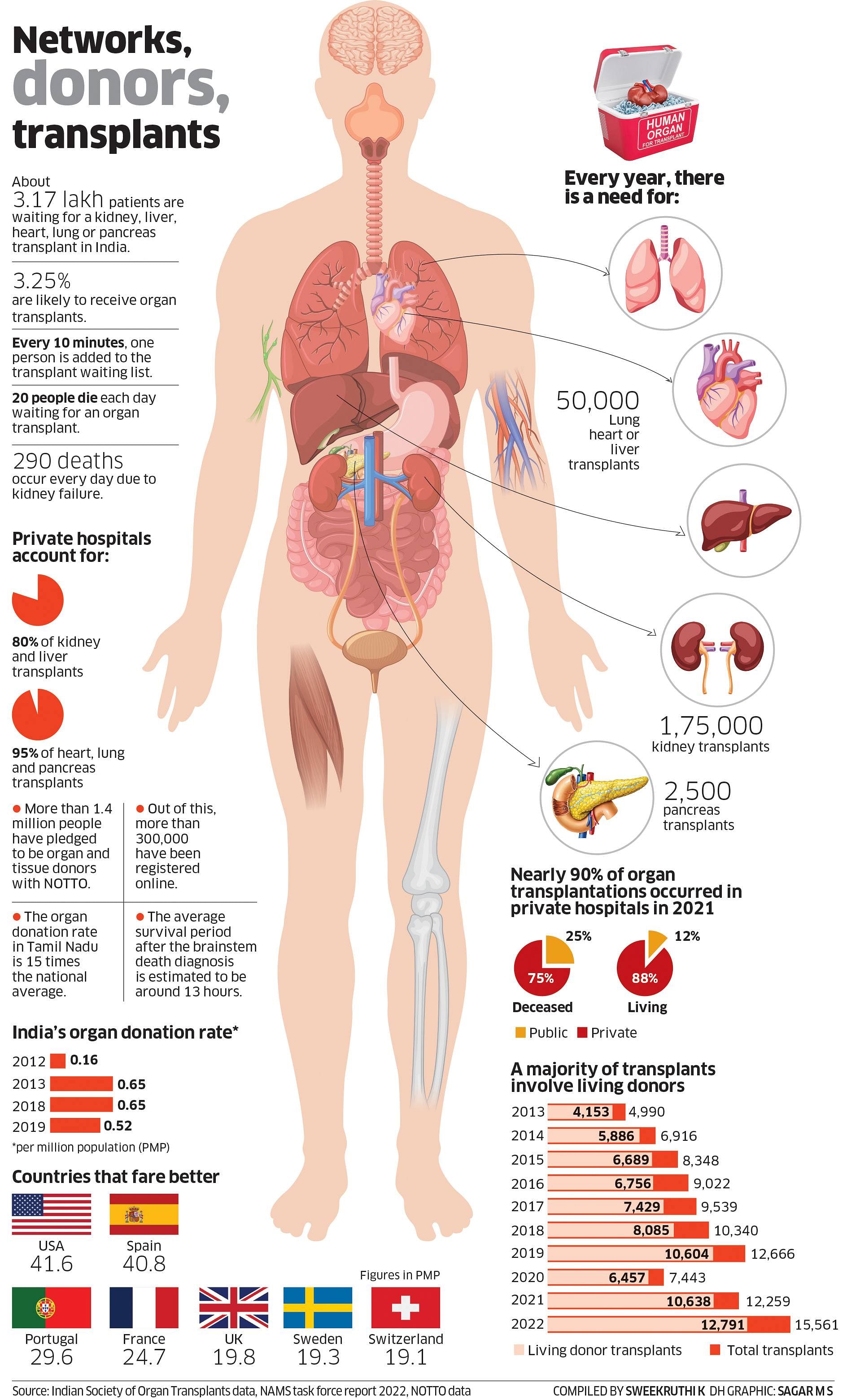
According to the National Organ and Tissue Transplant Organisation (NOTTO), there were 15,561 organ transplants in India in 2022, of which the overwhelming majority (12,791) were living donor transplants, mostly in private hospitals. Of last year’s 11,423 kidney transplants, 9,834 were from living donors. Similarly, out of 3,718 liver transplants, as many as 2,957 were living transplants.
In 2019, more than 95% of liver transplants were done in 175 private sector hospitals.
Even though transplants have tripled in the last ten years – from 4,990 in 2013 to 15,561 in 2022 – the number is still miniscule compared to India’s disease burden.
Against a requirement of one to two lakh kidney transplants, just about 10,000 such operations have taken place each year since 2019 (barring the Covid-affected 2020), mostly in metro cities. Similarly, Indian doctors conduct around 2,000 liver transplants against an annual need of 30,000 such procedures. The number of heart and lung transplants are in the hundreds, while pancreas transplants have never crossed the 50 mark.
What has caused such a situation? Why is it that big corporate hospitals have performed thousands of such surgeries – the Apollo group claiming 23,000 organ transplants in 11 years – but only a handful of government hospitals such as All India Institute of Medical Science, Delhi, and Post Graduate Institute of Medical Education and Research, Chandigarh, take up these surgeries?
“While we have enabling law in the form of the Transplantation of Human Organs and Tissues Act, 1994, we have not reformed the healthcare system,” said Dr Vivekanand Jha, executive director of The George Institute Global Health, India.
“There are no good incentives for public sector hospitals. In government hospitals, organ transplant is often not a priority,” Jha added.
High cost of such procedures, hospitals’ inability to convince the families of brain-dead patients to donate their organs and reluctance to allow organ harvesting due to religious and cultural reasons are factors restraining the availability of cadaver or deceased donations.
According to Dr Samiran Nundy, a gastro-intestinal surgeon at Sir Ganga Ram Hospital in Delhi and a pioneer of organ transplant in India, liver transplantation is an expensive procedure. It requires major investments in trained workforce as well as infrastructure in the form of supportive technology. The cost of a living donor partial liver transplant varies from Rs 16 to 40 lakh in private hospitals.
“In the public sector, there is no incentive given to surgeons and anaesthetists to spend long hours performing a liver transplant and then deal with the possible complications. Offering liver transplantation in a private hospital is a major booster to its reputation," he wrote in an editorial last year in the Journal of Clinical and Experimental Hepatology.
In Tamil Nadu, a state that began organ transplantation before others, only eight government hospitals offer kidney and liver transplant services as against 89 in the private sector. Karnataka has 68 hospitals registered as organ transplant centres whereas in India’s most populous state Uttar Pradesh, liver and kidney transplant surgeries are performed in less than 10 hospitals.
Cost is a big factor for UP’s poor track record. Post-operation expenses only add to the cost burden. “Following surgery, a person will have to shell out Rs 35,000 to Rs 40,000 per month on medicines to maintain their immunity. For somebody from a middle-income background, it is a huge amount because of which many prefer to live with their disease rather than bearing more financial obligations,” said Dr Mukesh Rai, a Varanasi-based surgeon who runs a private hospital.
Sharing his experience with kidney patients, Rai said while a transplant could add five to ten years to a patient's life depending on their co-morbidities, normal dialysis could also keep a person alive for seven to eight years. “Most of my patients suffering from kidney damage choose dialysis, even though taking all expenses into consideration, it roughly costs as much as a transplant.”
While Tamil Nadu, Telangana, Karnataka, Gujarat and Maharashtra traditionally have better track records on transplant surgery, the numbers rose sharply in Delhi-NCR in recent years, mainly due to well-equipped private hospitals.
Since 2008, when the Transplant Authority of Tamil Nadu was launched, as many as 9,087 organs have been harvested and transplanted in the southern state.
“More people wait for organs due to a demand-supply mismatch. We need to improve the brain death certification process, harvest the organs and distribute them,” said Dr J Amalorpavanathan, a renowned vascular surgeon who was the first convenor of the TN authority.
Other restraining factors include hospitals not hiring transplant coordinators and grief counsellors, hospitals not having specialists to certify a brain-dead patient and lack of adequate arrangements for the traffic police to transfer road accident victims quickly to hospitals.
Also, there is reluctance on the part of treating doctors to discuss the matter with the patient’s family, even though it has been estimated that there are at least four brain-dead donors (mainly after road accidents) in intensive care units every month.
Cultural beliefs
“The most difficult part is to persuade the family," noted Dr Abhijit Chandra, the head of the department of gastro-intestinal surgery at King George Medical University in Lucknow, who led a team of surgeons to perform the institute’s first combined liver-kidney transplant in November 2022.
Cultural and religious beliefs play a key role in people’s hesitancy for organ donation. “As per Hinduism, the last rites of a person are not permitted in a conventional manner if the body is 'violated' after death," said Alok Srivastava, a professor at Uttarakhand Ayurveda University, Dehradun.
A counter, however, comes from Dr Amalorpavanathan, who argued these were exceptions. “I remember two or three cases where people were hesitant due to cultural issues. One person told us he would come back after consulting the local temple priest but never came back. But these were mere exceptions."
He adds that people will come forward to donate if the need and process is explained properly. “But we need experts for brain-death certification and maintenance. We need professional coordinators to deal with families. It requires empathy to ensure that the families are not angered."
Trained professionals
Hemal Kanvinde from Multi Organ Harvesting Aid Network (Mohan) Foundation, an NGO that promotes organ donation, said there was a shortage of qualified medical staff at hospitals to certify brain deaths. "While larger hospitals have brain death committees, smaller hospitals do not have this facility at all,” she said.
The law requires four doctors, including the treating physician and a neurosurgeon as well as representatives of the hospital and government to certify brain death at two intervals, six hours apart.
“This is difficult to implement in a public hospital, where there is no incentive for these individuals to spend time doing this. Furthermore, presumed consent is not mandated in Indian law and the declaration of brain death is linked to the act of organ donation, an anomaly which contributes to hesitation on the part of treating/critical care teams to request a donation,” Nundy wrote.
Ideally, when a hospital identifies and certifies a patient as brain dead, they inform the State Organ and Tissue Transplant Organisation (SOTTO) with relevant details. The SOTTO's job is to identify the patients on the waiting list and alert the hospital concerned. But doctors said a lot needed to be done to improve the performance of these procurement organisations.
Transplantation programmes
"It is primarily the responsibility of the state governments to take steps for increasing deceased organ donation, develop infrastructure, provide workforce for organ donation and transplantation and monitor such deaths. The data regarding the number of deaths due to non-availability of human organs on time for transplantation is not maintained centrally," Satya Pal Singh Baghel, the Union Minister of State for Health, informed the Parliament earlier this week when asked about the lack of organs for transplantation.
The Union Health Ministry now plans a restructuring of the NOTTO as a part of which the national agency is working on a transplant manual. This will serve as a guide for implementation of organ donation and transplantation programmes in hospitals. A standard course for training of transplant coordinators is also being designed. Both these documents will be completed and released shortly. Four separate units for coordination, information sharing and awareness, training and human resources will also be created for better implementation.
“But unless some radical steps are taken, we are afraid things will remain as they are and have been for the last 30 years,” Nundy wrote.
(With inputs from Anand Singh in Bengaluru, E T B Sivapriyan in Chennai, Sweekruthi K in Bengaluru)
